If you’ve ever Googled “overtired baby won’t sleep” or “overtired baby keeps waking up,” you’re not alone! So many parents think their baby’s wakefulness is due to overtiredness, and it’s a common theory you’ll hear from sleep consultants, baby forums, and even some healthcare professionals. But here’s the kicker: overtiredness is not the sleep disruptor you have been led to believe it is.
In fact, overtiredness is not even a scientific term, and there’s no solid evidence linking it to the sleep problems we’re often told it causes. So, what is really going on when your baby won’t sleep? Could other factors like low sleep pressure or separation anxiety be the real culprits?
That’s exactly what I dive into in this mythbusting video!
This video is part of the BONUS Mythbusting Video Series included in my Baby Sleep Revolution™ program. It aims to help parents stress less about overtiredness — and figure out what might actually be going on instead. After watching it, you’ll feel more empowered to tackle your little one’s wakefulness with a clearer understanding of what’s likely to be causing it.
Watch the video for all the details! 👇 (or scroll down for the transcript)
[REFERENCE LIST + TRANSCRIPT BELOW]
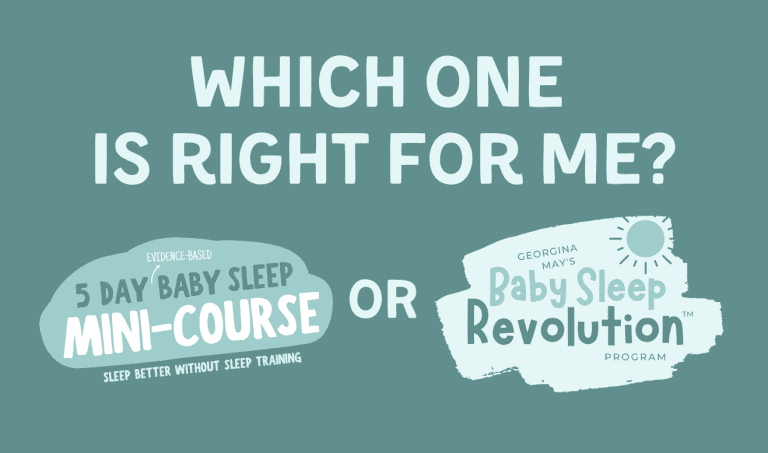
Struggling with wakefulness?
Here’s how I can help…

Discover the little-known secrets to improving sleep and settling …in less than a week!
This evidence-based (& highly effective!) course is for you if:

Help your VERY wakeful little one sleep soundly, for decent stretches at night, WITHOUT sleep training.
This one-of-a-kind program may be a total game-changer for you if:

References
- Adam, E. K., & Kumari, M. (2009). Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology, 34(10), 1423–1436. https://doi.org/10.1016/j.psyneuen.2009.06.011
- Harvard Medical School. (2024, April 3). Understanding the stress response. Harvard Health; Harvard Health Publishing. https://www.health.harvard.edu/staying-healthy/understanding-the-stress-response
- Berlin, L. J., Martoccio, T. L., Bryce, C. I., & Jones Harden, B. (2019). Improving infants’ stress-induced cortisol regulation through attachment-based intervention: A randomized controlled trial. Psychoneuroendocrinology, 103, 225–232. https://doi.org/10.1016/j.psyneuen.2019.01.005
- Howell, B. R., McMurray, M. S., Guzman, D. B., Nair, G., Shi, Y., McCormack, K. M., Hu, X., Styner, M. A., & Sanchez, M. M. (2017). Maternal buffering beyond glucocorticoids: impact of early life stress on corticolimbic circuits that control infant responses to novelty. Social neuroscience, 12(1), 50–64. https://doi.org/10.1080/17470919.2016.1200481
- Nachmias, M., Gunnar, M., Mangelsdorf, S., Parritz, R. H., & Buss, K. (1996). Behavioral Inhibition and Stress Reactivity: The Moderating Role of Attachment Security. Child Development, 67(2), 508–522. https://doi.org/10.1111/j.1467-8624.1996.tb01748.x
- Badanes, L. S., Dmitrieva, J., & Watamura, S. E. (2012). Understanding Cortisol Reactivity across the Day at Child Care: The Potential Buffering Role of Secure Attachments to Caregivers. Early childhood research quarterly, 27(1), 156–165. https://doi.org/10.1016/j.ecresq.2011.05.005
- Gunnar, M. R., Hostinar, C. E., Sanchez, M. M., Tottenham, N., & Sullivan, R. M. (2015). Parental buffering of fear and stress neurobiology: Reviewing parallels across rodent, monkey, and human models. Social neuroscience, 10(5), 474–478. https://doi.org/10.1080/17470919.2015.1070198
Transcript
Let’s talk about babies and ‘overtiredness’, and why you don’t need to worry anywhere near as much about overtiredness as you’ve been led to believe.
Overtiredness is a really common term. It’s everywhere. It’s used by parents, sleep experts, even some healthcare professionals. But here’s the thing. It’s not actually a scientific term. At its most basic, overtiredness is just an everyday word used to describe a situation where a little one is really tired, where they have really high sleep pressure, which would be fine if that’s all it was. But unfortunately, it’s often made out to be a major cause of sleep problems when it’s not.
As parents, we’re frequently told to keep a lookout for tired signs like yawning, or rubbing eyes or fussiness, and to put baby down as soon as we notice any of these ‘sleepy cues’ so we don’t miss the magic window and they become overtired. Because if they get overtired, they’re going to fall sleep or have trouble sleeping well – waking soon after we put them down, or sleeping really lightly, or waking frequently at night.
So, basically, we’re told that overtiredness, or very high sleep pressure, causes sleep problems like sleep resistance and wakefulness. But this isn’t true. From a sleep science perspective, there is zero evidence associating high sleep pressure with difficulty falling asleep, or delayed sleep onset or increased wakefulness. In fact, it’s the opposite. The more tired you are, the higher your sleep pressure and the more likely you are to fall asleep quickly and to sleep for longer or more deeply.
Now, sometimes a bit of a scientific explanation is also added, which can make this idea of overtiredness sound more legit.
Parents may be told that when their little one is overtired, their body will release cortisol, and that’s what affects or inhibits sleep: so – ‘overtiredness’ – or very high sleep pressure, leads to increased cortisol, which leads to sleep resistance and wakefulness.
Now, this is actually partially true. The last bit of it is. High cortisol can inhibit sleep. But tiredness or overtiredness is not what causes an increase in cortisol.
In fact, when you look at a chart, baseline diurnal cortisol levels in the body actually peak in the morning, just after we wake, and reduce over the course of the day, reaching the lowest level around bedtime. So as our sleep pressure is rising, our baseline cortisol level is actually falling [1].
But cortisol levels can increase at any time of the day if we experience stress. So when our brains perceive a threat, whether it’s physical or mental, it can activate the body’s stress response system – the sympathetic nervous system and the HPA axis – which triggers the release of cortisol, as well as adrenaline and other hormones that prepare the body for fight, flight, or freeze [2].
Stress makes it very difficult to sleep, which makes complete sense, because if the brain perceives you to be in some kind of danger, it’s not going to want you to sleep. It’s going to want you to do what’s necessary to feel safe again. So stress leads to increased cortisol, which can lead to sleep resistance or wakefulness.
Stress is a very common sleep disruptor for adults and older children, especially those who struggle with anxiety or a racing mind. For babies and toddlers, it’s more likely to be things like separation anxiety or stressful events – like starting daycare or the change of a caregiver or the arrival of a new sibling, things like that.
But when babies are very tired or ‘overtired’, are they likely to be experiencing a stress response? The answer is no. Unless, of course, they’re also experiencing some kind of stressful situation or event and their caregiver(s) are not responding to them. That can obviously trigger a stress response.
But it is absolutely possible for a little one who is very tired to be fussy, unsettled, or more emotionally reactive or dysregulated, maybe even have a bit of a meltdown. And that’s because tiredness affects the amygdala, the part of our brain that helps us to regulate our emotions. However research has found that when little ones are unsettled or upset, provided a trusted caregiver is responding to them – picking them up, soothing them, helping them regulate – they’re very unlikely to experience an increase in cortisol levels or a stress response [3-7]. This is also referred to as parental buffering, because by responding to baby, you’re helping them regulate their emotions and preventing a stress response.
Now, of course, if a little one is upset for any reason, it will probably take a little bit of time to help them calm down into a state where they can fall asleep. So, in that sense, an upset baby may take a bit longer to settle.
But in general, being overtired or having high sleep pressure doesn’t cause major sleep problems. In fact, it’s typically associated with faster sleep onset and longer, deeper periods of sleep. So you really don’t have to be too worried about overtiredness.
The bigger problem for most parents, especially if they have a little one who doesn’t need a lot of sleep, is usually the opposite: undertiredness. As in, trying to settle a little one when they’re not tired enough, when their sleep pressure is not high enough. Because if you do this, it can lead to sleep resistance – a little one who fights sleep – and/or an increase in wakefulness at night.
So the biggest takeout here is to be mindful that there are many possible reasons why a little one may be fussy or unsettled, and so it’s important to consider other likely causes – things like boredom (boredom is a big one!) separation anxiety or hunger – instead of just assuming a little one’s unsettledness is due to tiredness.
So that’s overtiredness! I hope this video has helped shed some light on this extremely common sleep idea, and you’re now feeling a bit more relaxed about sleep!